The United States has a well-established trauma system that designates each hospital to a tier and sends patients to the appropriate regional hospital based on their condition.1,2 Could a similar system be developed to better treat patients with sepsis?
Read the source article for this feature from
Critical Care Medicine.
Sepsis treatment and outcomes have improved since the Society of Critical Care Medicine and European Society of Intensive Care Medicine established the Surviving Sepsis Campaign in 2002.
3 However, sepsis remains the leading cause of death in U.S. hospitals, accounting for one-third of hospital mortality.
4,5
The risk-adjusted mortality from sepsis varies by 40% across hospitals,
6 said Nicholas M. Mohr, MD, MS, FCCM, professor of emergency medicine, anesthesia critical care, and epidemiology at the University of Iowa Carver College of Medicine. Dr. Mohr and his research team set out to determine whether creating a targeted regionalization sepsis network in the United States—similar to networks used for trauma and stroke—would improve outcomes. The study was published in the July 2025 issue of
Critical Care Medicine.
7
The Findings
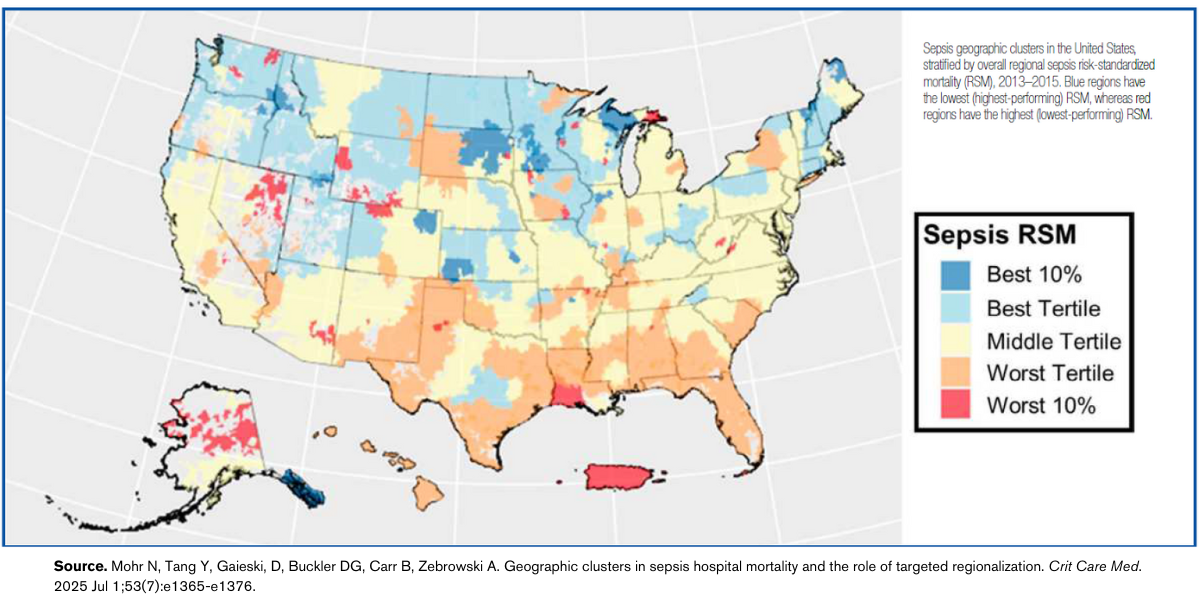
The researchers performed four simulation studies of strategies for sepsis patient reallocation using data from 1.12 million fee-for-service age-qualifying Medicare beneficiaries who were hospitalized for sepsis between January 1, 2013, and September 30, 2015. They developed geographic clusters to see whether targeted outcome-based regionalization could reduce preventable sepsis deaths.
Their primary performance outcome was survival to discharge. “Our hypothesis was that if we could identify top-performing hospitals and preferentially admit sepsis patients to those hospitals, that would be one way to use the healthcare market to improve aggregate sepsis care,” Dr. Mohr said.
The researchers were surprised by the finding that reallocation only minimally improved survival. “What we found was that even if we reallocated patients—we developed a regionalization system, ranked hospitals, and prioritized patients to go to certain hospitals—the improvement in aggregate sepsis outcomes was modest,” Dr. Mohr said.
All four simulations showed only small improvements in mortality, but all four showed increases in both patient travel time and sepsis volume at higher-performing hospitals.
In one simulation, 5% of sepsis patients were reassigned to the highest-performing hospital in the geographic cluster, but mortality in those patients decreased by only 1%. Averaged across the entire U.S. healthcare system, this would translate to only a 0.05% absolute sepsis mortality reduction. In addition, the reallocation increased the median distance from a patient’s residence by 35 miles and increased the volume in high-performing hospitals by 45%.
Another simulation reassigned 5% of patients starting from the lowest-performing hospital to the top-performing hospital. The reassigned patients had a 1.9% decreased absolute mortality.
“What we saw in our data was that moving people between hospitals is not likely to have a big benefit,” Dr. Mohr said. “Even if we can improve performance in the lowest-performing hospitals by 1%, that far outshines the benefit we would have seen from targeted regionalization.”
The study also found that hospital performance was highly correlated within a geographic region, Dr. Mohr said. Also, even if a sepsis system designated a higher-performing sepsis hospital, that hospital did not necessarily have the capacity to accept more patients.
What’s Next
The study findings suggest that overall sepsis outcomes are more likely to improve by focusing on quality care—determining why some hospitals perform better and using that knowledge to improve performance at all hospitals, Dr. Mohr said. His next research project will focus on examining these reasons. “We’re going to identify high-performing hospitals and characterize their performance improvement systems to try to understand what is portable, adaptable, and implementable in other hospitals,” he said, “because, based on the results of this study, we now think that’s where there’s more juice for the squeeze.”
Studying sepsis outcomes is part of a larger area of research into how healthcare systems can address overcapacity and variations in outcomes. Dr. Mohr wants to find solutions to this challenge. The results of his recent study emphasize how the strain on healthcare systems can affect a variety of acute care conditions.
“One of the things that we saw in this study was that reallocation in most cases would allocate more patients to hospitals than they have capacity to treat,” he said. “For the past 10 years, we’ve seen that tertiary care centers are more and more full, are more and more stretched, and the capacity to flex to changes in patient volumes has really been reduced.”