Paul E. Wischmeyer, MD, EDIC, FASPEN, FCCM, has a highly personal understanding of the challenges of recovering from an intensive care unit (ICU) stay. Diagnosed at age 15 with ulcerative colitis, his colon was removed when it perforated and caused septic peritonitis. Throughout his life, he has had 27 major surgeries and multiple ICU stays for bowel resections after bowel obstructions or to address complications from recurrent intestinal obstructions. These experiences have motivated his research to test a personalized, remotely monitored, coached exercise program to help patients recover after ICU discharge.
|

|
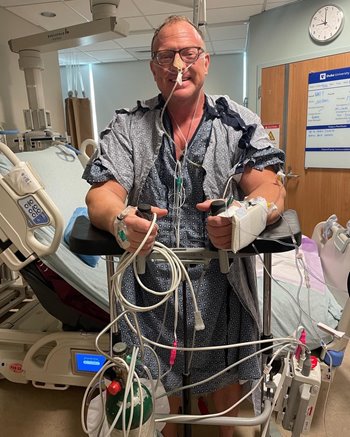
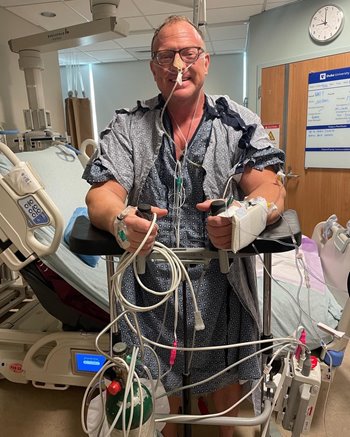
| Dr. Wischmeyer, four weeks before surgery, wearing a Bluetooth cardiopulmonary exercise test mask and performing the step test at study enrollment to assess baseline peak oxygen consumption while measuring heart rate to set limits for the high-intensity interval training. |
More than half of patients who spend time receiving treatment in the ICU experience post-intensive care syndrome (PICS) after ICU discharge. Symptoms include persistent neuromuscular weakness, exercise intolerance, and cognitive disfunction. Yet patients typically receive limited physical therapy and guidance to help them regain quality of life after ICU discharge.
Dr. Wischmeyer and his research team set out to determine whether a structured, personalized exercise program could improve patient outcomes. His pilot study received a 2021 Society of Critical Care Medicine Discovery Grant, which led to a $4.2 million National Institutes of Health (NIH) grant to conduct a multicenter trial. “One of the real challenges of rehabilitating from the ICU is, we tell patients it’s important for them to go home and exercise, but there’s virtually no guidance or support post-discharge. Maybe they’ve received some physical therapy in the hospital or they’ve been given exercise handouts, but they’re expected to do it on their own, and most people aren’t exercise experts or perhaps have never exercised at all prior to their illness,” said Dr. Wischmeyer, principal investigator (PI) for the study and professor of anesthesiology and surgery at Duke University School of Medicine in Durham, North Carolina. “Even if they go to a rehab facility, it’s a good start but it’s not necessarily going to get them where they want to be.”
|

|
| Jeroen Molinger, left, exercise physiologist lead for the study, and Ashley Artese, middle, one of the physical therapists for the study, performing baseline measurements on Dr. Wischmeyer, right, via ultrasound to assess muscle mass, muscle glycogen, and muscle quality. |
| |
The study will test the benefits of a novel, personalized, remotely monitored, mobile health-supported, high-intensity interval training (REMM-HIIT) exercise program with ICU survivors using wearable mobile devices (i.e., Apple Watches and iPhones given to patients). The REMM-HIIT concept was originally conceived during Dr. Wischmeyer’s work with Tony Sung, MD, a bone marrow transplant oncologist at Duke. Dr. Sung used the program to improve patients’ fitness before bone marrow transplant. He found that patients exercised more than requested and improved their cardiopulmonary fitness levels by more than 25% in four weeks. This led to the application for the SCCM Discovery Grant to study critically ill COVID-19 patients.The Discovery-funded pilot included 20 patients, enabling researchers to build a protocol, infrastructure, and a trial-specific app called SplendoFit that patients use to manage their personalized exercise programs. These patients will be included in the NIH-funded study. Their outcomes will be released when the study is complete. Enrollment for the NIH-funded study has begun and will include 140 patients who were treated for COVID-19, many of whom are at risk for developing long COVID. Study sites and PIs are shown in
Table 1.
Table 1. Study sites and PI(s)
| Study site |
PI(s) |
| Duke University Medical Center |
Paul E. Wischmeyer, MD, EDIC, FASPEN, FCCM
Amy Pastva, PT, PhD |
| Vanderbilt University Medical Center |
Matthew Mart, MD
E. Wesley Ely, MD, MPH, MCCM |
| Ohio State University Medical Center |
Nathan E. Brummel, MD, MSCI |
| University of Alabama at Birmingham |
Peter E. Morris, MD |
| |
 |
| Dr. Wischmeyer ambulating and starting his physical therapy in the ICU just a few hours after his initial 13-hour surgery. |
Patients will be randomized to receive either usual care (exercise handouts) or participation in the personalized exercise program. Both groups will receive an iPhone and Apple Watch to record their activity. Much like how professional and Olympic athletes guide their training, researchers in this study will determine each participant’s peak oxygen consumption via a Bluetooth cardiopulmonary exercise test mask and correlated heart rate to create a personalized high intensity interval training program targeted to the ability of each patient. A six-minute walk test, physical activity, and other measures, such as quality of life and cognitive function will be collected at enrollment as well. This information allows for creation of the individualized REMM-HIIT exercise programs for each patients. They will be coached through the app twice a week for three months by physical therapists (PTs) who are trained to facilitate ICU recovery, often the same PTs they worked with in the ICU and hospital during their stay. The program will be tailored based on what patients can do at home, including strength and balance exercises, sit-to-stands, and walking and/or bicycling.
Dr. Wischmeyer said personalization is key, since some patients work out regularly while others have never exercised at all. Holding them accountable and coaching them to stay in heart rate target zones via direct PT monitoring is critical, he said. “We’ll also be incorporating a range of basic science end points, studying mitochondrial function, which we think is a big driver of muscle function and recovery. Although we are studying COVID-19 patients, if the intervention proves valuable, we plan to study and implement it for use in all patients who spend significant time in the ICU.”
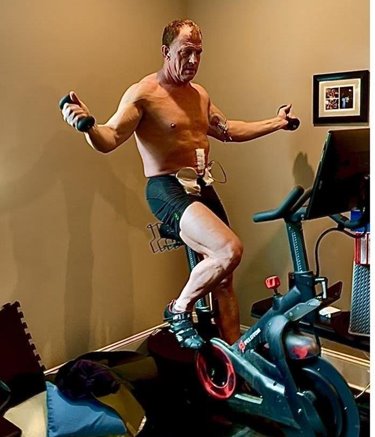 |
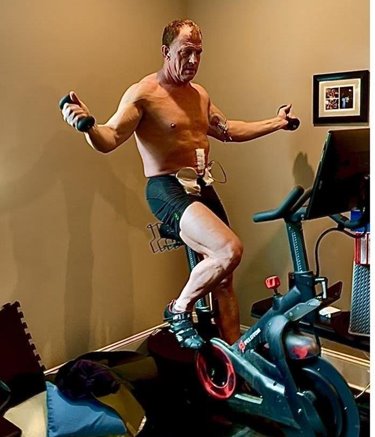
| Dr. Wischmeyer exercising at home one month after his ICU stay, even with open abdominal incision, abdominal fistula drain, and PICC line. |
Dr. Wischmeyer used several of the study’s exercise techniques himself when rehabilitating from a recent week-long ICU stay and time on mechanical ventilation after three major surgeries this past April. “My passion for medicine and improving care and outcomes for patients comes from my own experience with recovery from critical illness and surgery,” he said. “We would have never received this grant from the NIH without the essential pilot funding from the SCCM Discovery Grant. I am grateful for that seed funding, which led to what we hope will become a huge opportunity to create a personalized targeted ICU and COVID rehabilitation program that will be applicable not just in ICU patients, but also in patients as they prepare for surgery or cancer treatments.”
Discovery, the Critical Care Research Network
Discovery, the Critical Care Research Network, fosters collaborative research to improve outcomes for critically ill and injured patients and seeks to incorporate findings into practice using SCCM's broad base of programs.
Discovery Research Grants totaling $100,000 will be awarded annually to SCCM members as new pilot grants under the auspices of the SCCM-Weil Research Trust.
View more award recipients.
Post-Intensive Care Syndrome
Post-intensive care syndrome (PICS) consists of health problems that remain after critical illness. They are present when the patient is in the ICU and may persist after the patient is discharged. THRIVE is SCCM’s initiative to provide resources and education for ICU survivors and their families related to PICS.