The ICU Heroes Award recognizes that patients and families are an integral part of intensive care unit (ICU) care. The award is given to an ICU patient and family and to the multiprofessional team that delivered the care.
The letter was typed in gothic print, on a sheet of paper sandwiched between two handwritten notes, all in black except for a few brushes of pink and a pink heart at the top of the page. The words were poetic and heartfelt, bursting with gratitude. The letter was addressed to Nitin Puri, MD, critical care intensivist and division head of critical care medicine at Cooper University Health Care in Camden, New Jersey, USA, who, along with his care team and their patient, Jonathan Rosen, received the 2022
SCCM ICU Heroes Award. The letter was a show of admiration from a not-so-secret admirer, a love letter from the leader of the Love Army.
**********
“So many words of thanks to say to you. I will be sending them to you soon. For now, my deepest gratitude. You saved my husband’s life.”
Much of Jonathan Rosen’s adult life has been spent working in hospitals. He started in the trauma center at Cooper University Hospital when it opened in 1983. He went on to become an emergency medical technician, a nurse, a nursing and emergency department manager, and a regional sales manager for medical devices. At the onset of the COVID-19 pandemic, he wanted to put his nursing expertise to good use, so he took a position as a night nursing supervisor at a nursing facility. In that role, he visited every patient room in the facility and had direct contact with every staff member, monitoring them for COVID-19.
In April 2020, Mr. Rosen had the worst headache of his life while working the overnight shift. The next morning, he was tired and still had the headache in addition to fever and chills. For the next 10 days, he focused on breathing deeply, staying hydrated, and taking acetaminophen/paracetamol every six hours. “With each day, it became harder to lift my head or get out of bed,” he said. “I stopped eating and then stopped drinking fluids. If I did get up, I would become nauseous.”
On April 24, 2020,
he went to Cooper, where he expected to receive some fluids and be sent home. Instead, he was told his oxygen level was too low and he was admitted. On April 27, his oxygen level was not improving and he was started on mechanical ventilation. The last thing he remembers before being intubated was seeing the medical team. “I turned to someone near me and asked who they were,” Mr. Rosen said. “They said, ‘anesthesia.’ I laid my head back as they gave me IV sedation, and that was it, until I woke up in June.”
**********
“Thank you for your first-rate medical expertise, dedication, and professionalism at this extraordinary time. As well as the stellar care that Jonathan is receiving from you, we appreciate the extra kindness, hand-holding and updates you give every step of the way.”
In the early days of the pandemic, Cooper University Hospital had so many COVID-19 patients with acute respiratory distress syndrome that they created an auxiliary intensive care unit (ICU) on the hospital’s eighth floor. It was there that Dr. Puri first met Mr. Rosen, during a consultation to determine whether extracorporeal membrane oxygenation (ECMO) was warranted.
The consultation was brief. “It was very clear he wasn’t going to survive unless he got on ECMO,” Dr. Puri said. Dr. Puri spoke with Mr. Rosen’s wife, June, and had the “gut-wrenching” consent conversation. He told her that, because of the limited number of ECMO machines and the high number of patients who needed them, her husband would need to be removed from ECMO after a certain amount of time if his condition did not improve.
June told Dr. Puri not to worry. Her husband would get better. Initially, her prediction was right. His oxygen level did improve. Then one night, he began coughing up blood. Before long, there was blood everywhere. His endotracheal tube was occluded with blood and had to be replaced. His blood thinners were discontinued. Not long after that, the team discovered a large blood clot in the inferior vena cava. Typically, blood thinners would be administered to prevent the clot from spreading, but the team worried about the effects of blood thinners on him. “It was like he had a ticking time bomb in him,” Dr. Puri said.
Ultimately, blood thinners were started again, and that decision proved to be the right one. Mr. Rosen spent 58 days in the ICU, 24 of those on ECMO. He went to sleep in April and woke up in June, unaware of the pandemic’s status or any other news. All he had was a collection of vivid dreams. “So much happened during that time,” Mr. Rosen said. “I slept through it all and was not there, leaving my wife to manage everything alone, including me.” What he did not know was that his wife was not alone.
**********
“Whether you are explaining complicated medical procedures, educating me on best options for treatment, or stepping in as surrogate family to support Jon, I deeply appreciate your undivided attention, keen focus, and genuine humanity. It means the world to me.”
Hospital regulations prevented June from visiting her husband, so she communicated with his care team instead. They made sure she always received the latest news about his condition. June in turn shared this information with a network of family and friends, who began calling themselves the
Love Army. A website was launched with updates on his condition. Mr. Rosen said that the site was accessed by more than 700 unique logins and viewed more than 25,000 times.

At first, the Love Army was there to support the Rosens but, thanks to June, they soon began supporting the Cooper care team as well. June wanted the entire ICU team to know that they were valued, appreciated, and loved. “There was no true Love Army without the extraordinary Cooper team,” June said. “Recognizing the gift of having dedicated, highly skilled professionals who were so genuinely kind and loving and battling to save those with COVID-19 on the front lines was the essence of our powerful Love Army.”
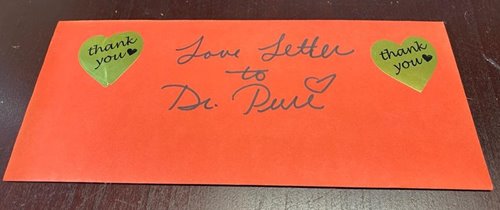
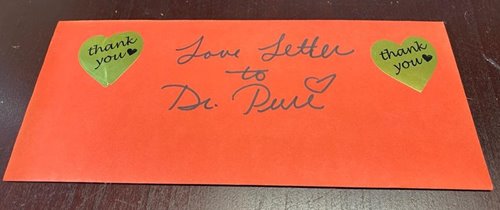
June told the Cooper team all about the Love Army—how it spanned the country, how it was staying current on Mr. Rosen’s latest condition, and how it was continuing to send well wishes to them, the caregivers. She got to know the nurses through their daily updates and wrote letters of thanks to dozens of people on the Cooper staff. She told them that they too were members of the Love Army. Her love letter of thanks to Dr. Puri is still easily accessible in his office.
That inclusion meant more than even June could know. “We went from these ecstatic highs to these dark, dark lows,” Dr. Puri said of the early months of the pandemic. ‘‘The number of lives lost was more than I ever could imagine. [June] gave back a lot to us, and we remain grateful to her and her family.”
**********
“I join with family and the ‘Love Army’ of dear friends to thank you for saving Jon’s precious life. You are a hero! With profound gratitude, appreciation, and much love.”
Mr. Rosen’s recovery process was long but not insurmountable. He lost 50 pounds in the hospital and could not walk, talk, eat, or swallow after being weaned from the ventilator. He underwent inpatient and outpatient rehabilitation, and started working out at a gym. He
continues to undergo muscle therapy and is being treated by a psychologist.
That is the hard work. What is easy is following his wife’s footsteps and showing appreciation to the Cooper care team. Mr. Rosen witnessed the risks physicians, nurses, and the entire team took to protect patients and the general public. He owed them his life and his gratitude. He keeps in
close contact with many of those who risked their lives to save him. He is an anchor of the hospital’s peer support survivor group and is an inspiration to the care team. Dr. Puri says that Mr. Rosen is now an essential member of the Cooper community.
“I have found that the best way I can thank them is by showing up or staying in contact so they can see me now, walking, talking, strong, and standing tall,” Mr. Rosen said. “I watch the joy and tears as they see me, and I like to think that my visits or connections show them that what they do matters.” This past fall, he had coffee with a Cooper physician, who broached the idea of participating in an Ironman Triathlon as a doctor-patient team. While this physician routinely competed triathlons, Mr. Rosen did not. After talking it over, the two came to a compromise—they would do a half-triathlon together. That consists of 1.2 miles of swimming, 56 miles of bicycling, and 13.1 miles of running. Mr. Rosen is currently training for the event.
Why would he take on such an immense physical and mental challenge? He said the answer is simple. “My reason for saying yes is to show those recovering, like me, that they too can get here, to honor the 875,000 who no longer can and for all those healthcare workers like my team at Cooper, to show them that what they do makes a difference.”