The risk of death for patients with out-of-hospital cardiac arrest (OHCA) is high. Only about 20% reach the hospital alive. Among those who reach the hospital, short-term mortality can be up to 65%.1
Read the source article for this feature from
Critical Care Explorations.
It is critical to be able to assess prognosis soon after a patient is admitted to the hospital. Thevathasan et al developed a simple risk prediction score for patients with OHCA based on prospective data. Their study was published in the March compendium of
Critical Care Explorations.
2
“We developed this score to have a pragmatic tool that is not based on sophisticated calculations where you have to take time to actually calculate the risks,” said lead author Tharusan Thevathasan, MD, a critical care specialist in the Cardiology Department of the German Heart Center of the Charité University Hospital in Berlin, Germany, and research coordinator of the Berlin Cardiac Arrest Center at Charité University. “It’s a pragmatic, simple point-by-point score. It’s validated internationally, and it is based on granular, randomized data.”
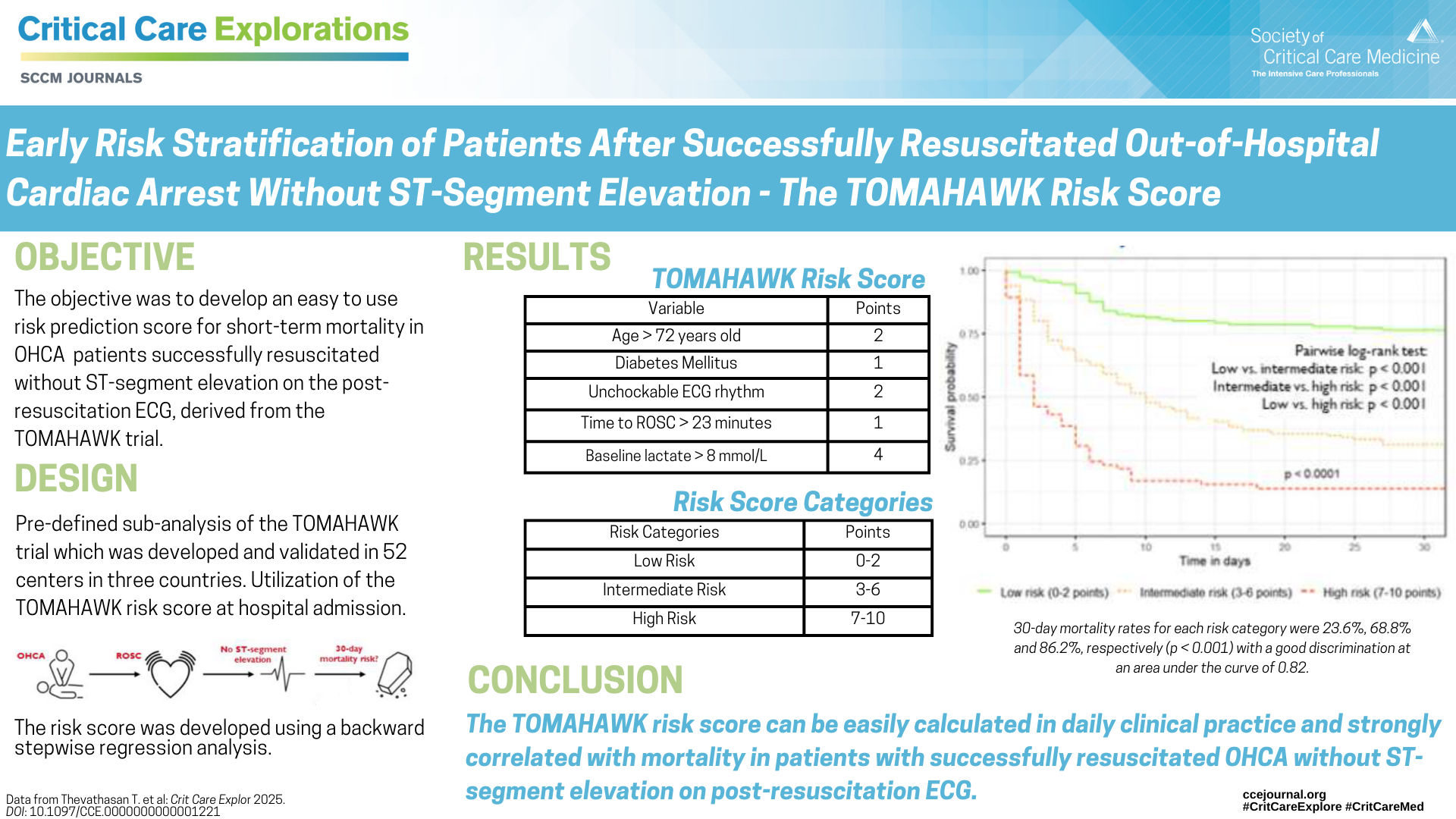
The risk score was developed based on data from the randomized controlled trial Angiography After Out-of-Hospital Cardiac Arrest Without ST-Segment Elevation (TOMAHAWK) across 31 hospitals in Germany and Denmark. It was then validated on randomized data from the Coronary Angiography After Cardiac Arrest Trial (COACT) across 19 hospitals in the Netherlands and Germany. Most current risk scores were built on registry or retrospective data and validated in only one country, said Dr. Thevathasan.
The risk score allows clinicians to assess prognosis within hours after hospital admission. “While final neurologic prediction is not recommended in the first three days, it is still helpful to stratify risk to inform treatment decisions, allocate resources, speak with family members, and standardize post-resuscitation medical care,” said Steffen Desch, MD, an interventional cardiologist at the Heart Center of Leipzig in Leipzig, Germany, and senior author of the article. “Our tool is not as accurate as the standard prognostic assessment after 72 hours or later, but it comes very close.”
The Findings
The risk score was developed using a backward stepwise regression analysis. Five variables surfaced as independent predictors of 30-day mortality. The five variables were given weighted points based on risk, and three categories were created to assess risk:
- Low (0-2), with 23.6% risk of 30-day mortality
- Intermediate (3-6), with 68.8% risk of 30-day mortality
- High (7-10), with 86.2% risk of 30-day mortality
The five variables are:
- Age 72 or older = 2 points
- Known diabetes = 1 point
- Unshockable initial ECG rhythm = 2 points
- Time until return of spontaneous circulation (ROSC) greater than or equal to 23 minutes = 1 point
- Admission arterial lactate level greater than or equal to 8 mmol/L = 4 points
These five variables matched up with what physicians see clinically. “Arterial lactate has been known for decades as a marker of adverse prognosis; so has the time until the patient is no longer dependent on resuscitation and unshockable ECG rhythms,” Dr. Desch said. “Age is self-explaining, and diabetes could be seen as a general measure of high comorbidity burden or poor health status to begin with.”
Diabetes has not been included in previous risk scores, but with the TOMAHAWK risk score, the impact of diabetes on prognosis was as strong as time until ROSC. The TOMAHAWK risk score is not a standalone tool; it is meant to supplement clinical judgment.
Dr. Thevathasan said the variables are intuitive to clinicians, but adding up the points helps them stratify scores for individual patients. “It’s always interesting to see where the patient is regarding the extremes—are they at the bottom or at very high risk?” he said.
What’s Next
Future steps may include a more detailed analysis of post-ROSC patient characteristics after OHCA to improve early risk stratification. “Combining the use of AI to interpret ECG patterns with early sequential assessments of biomarkers and clinical trajectories offers the potential to quantify individual patient risk more precisely,” Dr. Desch said.
References
- Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020 Feb 22;24(1):61.
- Thevathasan T, Spoormans E, Akin I, et al. Early risk stratification of patients after successfully resuscitated out-of-hospital cardiac arrest without ST-segment elevation: the angiography after out-of-hospital cardiac arrest without ST-segment elevation (TOMAHAWK) risk score. Crit Care Explor. 2025 Mar;7(3):e1221.