Guideline for the Treatment of Heat Stroke
Citation: Barletta JF, Palmieri TL, Toomey SA, et al. Society of Critical Care Medicine guideline for the treatment of heat stroke. Crit Care Med. 2025;53(2):e490-e500.
Predicted increases in heat-related weather phenomena will result in increasing heat exposures and heat injuries such as heat stroke. Prompt recognition, early intervention, and evidence-based management are necessary to optimize outcomes. These SCCM guidelines outline recommendations for the treatment of patients with heat stroke.
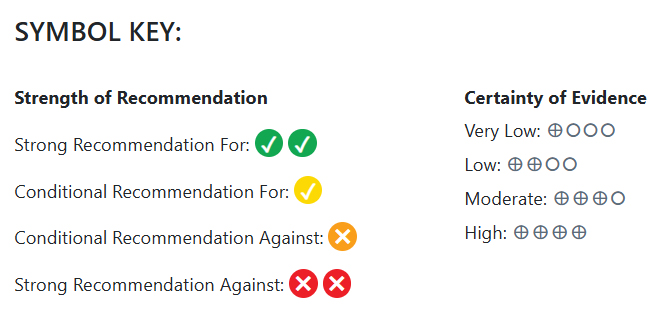
The guidelines panel generated two strong recommendations, five good practice statements and one “only-in-the-context of research” statement. Active cooling measures are recommended over passive cooling methods, with cold- or ice-water immersion achieving the fastest cooling rate. This method should be prioritized where available. In patients with heat stroke, there is no evidence to support pharmacological interventions that affect temperature control, so they should be avoided.
Guideline Type: Clinical
Related Resources:
Executive Summary: Treatment of Heat Stroke
 |
Infographic: 2025 SCCM Guideline for the Treatment of Heat Stroke |
Section:
Strength:
Identifier:
We recommend active cooling methods over passive cooling in patients with heat stroke.
Certainty of Evidence: Very Low
Clinicians should prioritize cooling methods that achieve the most rapid rate of cooling. This includes ice-water immersion (1-5 °C) or cold-water immersion (9-12 °C).
Clinicians may use similar strategies for either classic or exertional heat stroke.
Clinicians should choose cooling methods that reach the target temperature within 30 minutes from recognition of heat stroke symptoms.
Clinicians should prioritize cooling modalities that achieve a cooling rate greater than or equal to 0.155 ° C/min.
We recommend against the use of dantrolene in patients with heat stroke.
Certainty of Evidence: Very Low
The routine use of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDS), and salicylates for temperature reduction should be avoided.
Prophylactic antibiotics or prophylactic antiseizure medications should only be used in the context of research.